

One Year Later, Many Have Persistent Hearing LossĪll patients expressed concern about hearing loss or tinnitus (ringing in the ears). Patients with larger ruptures required surgical repair, which had a high rate of success (86 percent). In 38 percent of cases, the perforations healed spontaneously.

Rates of perforations were nearly three times higher for patients who had other significant injuries related to the bombings, and for those who were closer to the blast. Overall, 90 percent of patients hospitalized for other injuries had tympanic membrane perforations on examination. The most common type of otologic injury was tympanic membrane perforation, which is a ruptured eardrum.įorty-eight patients had tympanic membrane perforations, with 14 patients having perforations in both ears.
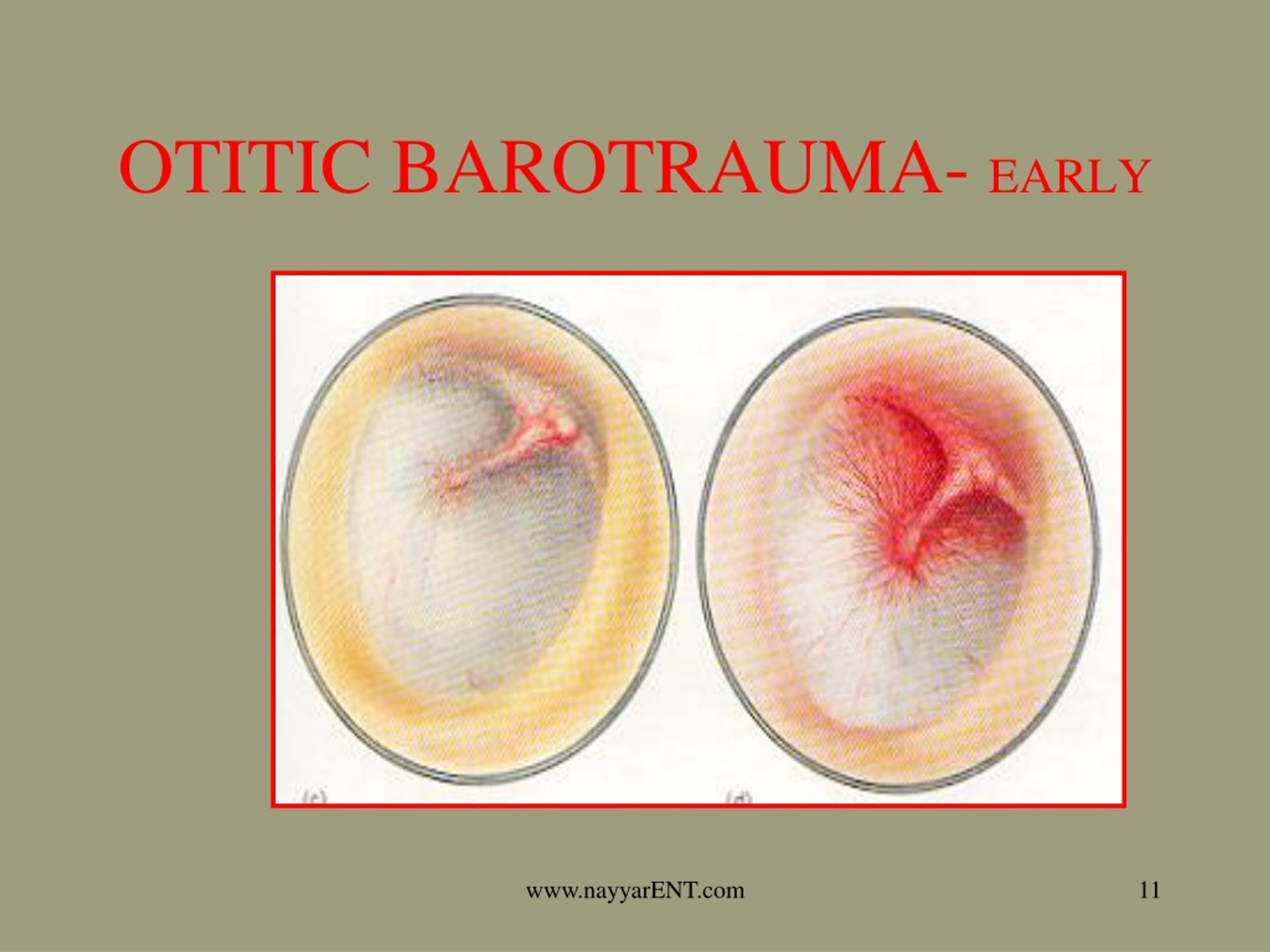
Most of the patients sustained primary blast injury known as barotrauma. Only seven percent of patients had any hearing-related symptoms before the attack. The study included 94 of the more than 100 patients evaluated at Boston area hospitals and clinics after the blasts, including: “However, the extensiveness was not appreciated until the days and weeks that followed.” Aaron Remenschneider, on of the principal investigators. “Acute otologic trauma following the dual blasts was immediately apparent,” said Dr. The study assembles data from eight hospitals that provided care for patients with otologic trauma caused by two bomb explosions near the finish line of the 2013 Boston Marathon. The researchers conclude, “Blast-related otologic (ear and hearing-related) injuries constitute a major source of morbidity following the Boston Marathon bombings.” Ruptured Eardrum and Other Injuries after Marathon Bombings Based on the O'Neill Grade assigned, evidence supported suggestions for appropriate actions and medical interventions are offered.After the Boston Marathon bombings, more than 100 people were treated for trauma affecting the ears and hearing–with many having persistent or worsening hearing loss or other symptomsĪ Boston-wide research collaboration has reviewed the experience with hearing injuries caused by the 2013 attack, including follow-up evaluation of hearing and related outcomes. We describe a newer grading system, the O'Neill Grading System (OGS), which allows simple, practical and consistent classification of ETD and MEB by all members of the clinical hyperbaric medicine team. It is not a practical tool for the modern hyperbaric team. The Teed's classification was not intended to correlate with the consistency of diagnosis, the clinical approach to relieving symptoms or the treatment of the inflicted trauma. Results from these examinations are used to determine the proper course of treatment for the ETD or MEB. Repeat otoscopy is required for patients having ETD, pain or other symptoms during the compression and/or decompression phase of the treatment. Currently, the standard of care is a baseline otoscopic examination performed prior to starting HBO2 therapy.

The current grading system, the Teed's Classification, was first described in 1944 with modifications to this system over the years, but none are specific for the evaluation and treatment of patients undergoing clinical HBO2 therapy. Eustachian tube dysfunction (ETD) and middle ear barotrauma (MEB) are the two most common complications of clinical hyperbaric oxygen (HBO2) treatment.


 0 kommentar(er)
0 kommentar(er)
